Introduction:
I don’t think there is anything that puts more fear in a caregiver when it comes to the matter of dysphagia than that around the topic of aspiration. Understandably so as aspiration events can lead to pneumonia and the ensuing complications which aspiration can cause.
Individuals with dysphagia having a varying degree of risk for aspiration. Some individuals have a low risk for aspirating in spite of their swallowing disorder. And of course, some individuals have a high risk for aspirating.
For the caregiver, understanding what their persons potential risk is for aspiration is important information so you can regulate the amount of fear and worry you should reasonably have. Knowing the risk factors your loved one has will guide you on how best to mitigate the risk.
The goal of this blog post on aspiration is to impart knowledge and education to empower caregivers on this topic. You will learn what aspiration is, the signs and symptoms to monitor for, and how to decrease the risk of aspiration at home.
There is a free printable guide available at the end of this post for you. I would recommend you have a copy available for all persons that provide care for your loved one to read. This will give them a better understanding of aspiration when caring for your loved one with dysphagia at home.
1: Understanding Aspiration and Dysphagia
In simple language, aspiration is when something goes down the wrong way or wrong tube and into your lungs by accident. There are multiple reasons or causes for this to happen. A person can aspirate on vomit, their own secretions, food, drink and any foreign object.
Once we swallow there are several actions that take place designed to protect our airway from having anything foreign go down this tube. The tongue base retracts and helps close off spaces, the epiglottis folds over the glottal space, our vocal folds close or adduct, and the larynx rises. This is a very simplistic description of the highly coordinated reflexes necessary to protect the airway.
As you can imagine a swallowing disorder in any of the three phases of swallowing can have a negative impact and consequences for airway protection and increase the risk of aspiration. Aspiration can lead to serious health issues such as pneumonia.
Aspiration does not always have a lot of symptoms. Aspiration can be “silent” meaning there are reduced symptoms or no symptoms or indication that something has gone down the wrong tube.
Aspiration pneumonia can happen days after the event.
Caregivers should always be alert and monitor for general symptoms if their loved one has dysphagia. However, they need to pay extra close attention for several days, at least seven days, if they have concern that an aspiration event may have occurred.
If you feel there has been an aspiration event or your loved one is not behaving in their normal pattern it is pertinent to make their Pcp aware. Your medical care team can assist making medical decisions if it is wise to go to the emergency room or to your Pcp office for further assessment. These can be hard calls to make and will help decrease your burden of worry and stress by notifying your physician sooner rather than later.
Your healthcare provider should be contacted immediately or go to the emergency room or call 911 if you’re loved one is having difficulty breathing.
2: How To Calculate Your Loved Ones Risk For Aspiration
Ideally you will have a speech language pathologist involved in your loved one’s care. A speech therapist can evaluate current swallowing function and skills at home. There are several areas to assess and take into consideration when evaluating a persons swallowing ability that gives the therapist an impression of the risk for dysphagia and aspiration.
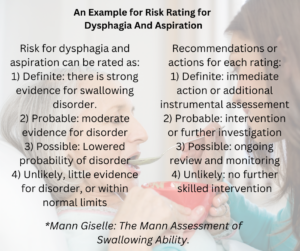
A speech therapist may use a tool such as The Mann Assessment of Swallowing Ability shown here during the swallowing assessment. This guides the therapist into what level of severity a person potentially presents and what action should be considered or taken.
A speech language pathologist is going to take a lot of factors into consideration when assessing an individuals risk factors for dysphagia and aspiration.
We will review pertinent recent, current and past personal medical history via medical records. Interview patient and caregivers about current and past signs and symptoms of dysphagia; history of dysphagia and/or aspiration and pneumonias; and reason for the current referral for a swallow evaluation.
The box on the left are areas of interest or concern that I address during a swallow evaluation.
You can take these points into consideration when you are thinking about your loved one’s current situation.
These are topic areas to discuss with your Speech Pathologist, PCP and medical team to help determine current aspiration risk and management decisions.
3. Techniques to Reduce Aspiration Risk:
The ultimate goal of all this information on dysphagia and aspiration is to make your loved one safer when eating and drinking. The caregiver plays a very important role in supporting and/or setting up your loved one for success at home.
 There are general practical steps to help prevent or reduce the risk for aspiration. A speech therapist may call these safe swallowing strategies. Again, these are general strategies that would make most any person safer when swallowing liquids or solids.
There are general practical steps to help prevent or reduce the risk for aspiration. A speech therapist may call these safe swallowing strategies. Again, these are general strategies that would make most any person safer when swallowing liquids or solids.
A speech therapist would individualize safe swallowing strategies for your loved one based on diagnostic assessments done or swallowing re-assessments done at each visit. So not all of these strategies are necessary for each person with dysphagia.
4. Creating a Safe Eating Environment At Home:
A) A low stimulus environment
Mealtimes should be as enjoyable and relaxing as we can make them. Some of our loved ones require a low stimulus environment in order to focus and pay attention to eating and drinking while using their safe swallowing strategies required to be safe. Take a look at all of the distractions in the environment and try and lessen them at mealtimes.
These can be visual distractions like too many items in the area where they are eating that they may focus on and move around. There could be visual distractions from a tv going and a show they are interested in watching vs. focusing on their meal. Pets can be visual distractions and be bothering the individual while they are eating. People coming in and out of the room while they are eating can be distracting and break a persons focus on what they are supposed to be doing.
Auditory distractions may be present with noise from other people or pets in the home. People on the telephone or talking with other people may make the person want to participate in what they are talking about than on eating their meal. Having the noise from a tv blaring, loud music playing, company talking or noises outside can all contribute to less attention to eating or drinking.
B) Proper Seating For Safer Swallowing and Conservation of Energy
This is a pet peeve of mine! Where a person sits to eat meals can make a huge difference in how safe they are consuming their food and liquids. A supported upright position also requires less work for an individual to consume a meal.
However, it is a challenging area to address as many folks today do not eat their meals at a table. Most common today is eating in the living room and most often in a recliner type chair. This poses a challenge for proper seating to decrease signs and symptoms of dysphagia and lower the risk for aspiration.

Optimal seating when consuming food or liquids is when seated on a firm surface. All joints should be bent or flexed vs. in extension. Head upright looking straight ahead and bent slightly forward; hips
flexed forward or at least upright at a 90 degree angle; and ones knees and ankles bent vs. being extended out. Their feet should be flat on the floor. Both forearms are able to rest on the table or on arm rests with elbows bent.
If your loved one is bed bound or eats and drinks while in bed, use of a wedge pillow and other supports (even with a hospital bed) will be needed to aid in lifting person up to the most upright position that can be achieved.
Positioning can be challenging in some situations due to the weakness, fragility, and severity of a persons illness. Have a discussion with your health care providers if you are unsure of how to position your loved one. It may be beneficial to have an occupational therapist evaluate for medical equipment needs for chairs, wheelchairs and or beds.
5. Emotional and Practical Support for Caregivers:
Many a time I have heard people say to me, “of course I know how to eat or drink I’ve been doing it my whole life and I don’t need a speech therapist for that!” This happens more often that you would think that individuals and their caregivers have no idea how significant dysphagia is to their well being and safety to staying healthy. They often want to refuse the referral to speech therapy for a swallowing assessment and treatment. They will need convincing or education that we are the profession to help with swallowing. Sometimes speech therapy is the key to keeping an individual at home and out of the hospital.
We are not used to having to pay close attention to when we swallow, eat or drink. We have swallowed our whole lives with the great fortune of not having to think about our safety when we eat or drink. It may take education and teaching to get an individual to “buy into” the recommendations for diet modifications and/or safe swallowing strategies made to them.
I try and encourage the person that is not following any of the recommendations at home to try for a trial period of one week as an assessment period. This way the reluctant individual can agree to a short period of time and not be overwhelmed thinking this is going to be for the rest of his life. During this period, the therapist, the individual and the caregivers can observe and assess the presence or decrease in signs and symptoms of dysphagia or aspiration when following a modified diet and/or while using compensatory safe swallowing strategies.
This amount of time gives the individual and the caregiver time to see if there are any benefits and improvements by following the recommendations. Often, the individual will see that they do make a difference in decreasing the signs and symptoms. Then we have a better chance of compliance or a least an individual willing to accept some of the changes recommended.
Caregivers can get frustrated with their loved ones when they do not take it seriously. In my experience, many times, people need time to adjust to the changes and start with baby steps and build on this foundation of willingness to try and implement some of the recommendations to manage their dysphagia and risks for aspiration.
Caregivers take on a lot of the worry, stress and anxiety as often their loved one is dependent on them for preparing the food and providing the meals. So caregivers feel responsible if their loved one is not accepting the changes or if their loved one gets sick with pneumonia.
I remind caregivers that they can only do the best that they can with the knowledge and information they had at the time and with the cooperation and willingness of the loved one to work with them.
Conclusion:
Some of our loved ones are at the end stages of chronic diseases, progressive diseases and/or battling acute and new health issues. Some times the risk of aspiration, pneumonia and dysphagia are going to be very high and probable and not responsive or lessened with any strategies we use.
If you are struggling and feel you or your loved one needs more support and assistance or assessments in the area of eating and swallowing, please request from your primary provider a new referral for speech therapy. Many times there are small modifications that can be made that may make a world of difference.
If you would like a free pdf printable on managing aspiration at home, you can get it here: https://thepureedkitchen.com/freebies/
Please leave an email if you have further questions and I’ll try and help!
You are doing a great job my friend.
Best wishes, Jean


